- A preoperative CT scan will show the site, severity, and extent of the airway compromise to assess the level and degree of obstruction.
- Assess the vocal cord function preoperatively
- Lung function tests to look for the extent of intrathoracic or extrathoracic obstruction.
- ECHO to rule out pericardial effusion and cardiac compression.
- Premedication with benzodiazepine is generally avoided if there is risk of airway compromise.
- Airway equipment—rigid bronchoscopy and difficult airway trolley, jet ventilation, cardiopulmonary bypass (CPB) should be there as standby. Femoro femoral bypass is the most common setup.
- COMPLICATIONS DUE TO MASS EFFECT OF THE TUMOUR:
- Vascular compromise—SVC Obstruction ( SVCO ) and pulmonary vessel obstruction
- Laryngeal nerve palsy
- Dysphagia
- STRIDOR and airway compromise may be an important symptom
- Inspiratory stridor (laryngeal)—obstruction above the level of glottis
- Expiratory stridor (tracheobronchial)—obstruction in the intrathoracic airways
- Biphasic stridor—obstruction between glottis and subglottis or a critical obstruction at any level
- Sometimes you may have to go for a microlaryngoscopy tube (MLT)
- TAKE CARE:
- Aim to avoid worsening of cardiac compression, airway occlusion, and SVC obstruction.
- IV cannula in the lower extremity
- Induction in sitting position (semi Fowler’s position)
- Inhalational (preferred choice) or IV induction agent titrated to effect
- Choose spontaneous ventilation with LMA
- Awake fibreoptic technique if intubation is necessary with a reinforced smaller calibre and longer endotracheal tube
- Postoperative airway obstruction due to airway oedema, tracheomalacia, and bleeding warrant the need for awake extubation in ITU. The following steps would aid in an uneventful extubation:
- Test for leak around the endotracheal tube cuff.
- Administer dexamethasone or chemo radiotherapy in sensitive tumours to shrink size of tumour.
- Use adrenaline nebulisers.
- Extubate over airway exchange catheters.
- SVCO: challenges during anaesthesia
- Need for supplemental oxygen
- Orthopnoea—induction in the sitting-up position
- IV cannula in the lower extremity
- Airway oedema
- Mucosal bleeding
- Laryngeal nerve palsy
- Haemodynamic instability due to decreased venous return
- OTHER CONCERNS
- General anaesthesia, causes loss of intrinsic muscle tone, decreased lung volumes, and decreased transpleural pressure gradient
- Positive pressure ventilation, can precipitate severe hypotension and also increases intrathoracic tracheal compression
- Coughing, as it can cause complete airway obstruction by positive pleural pressure, increasing intrathoracic tracheal compression
- Following gas induction, the patient stops breathing and if you are unable to ventilate her: Follow difficult or failed intubation guidelines. But cricoid puncture and emergency tracheostomy are futile if the level of airway obstruction is at the intrathoracic tracheobronchial tree: Try a change in position—lateral, sitting up, or prone—to decrease the mechanical effect of the tumour. Avoid positive pressure ventilation for fear of luminal closure. Low-frequency jet ventilation with Sander’s injector or high-frequency translaryngeal jet ventilation with Hunsaker’s catheter is one option. CPB bypass and ECMO to restore oxygenation when other measures fail.
- Following chemotherapy in ICU, if patient develops hyperkalemia, Tumour Lysis Syndrome should be there in the differential diagnosis
- ALSO NOTE
- During inspiration, the intrathoracic airways expand along with the expanding lungs. In contrast, the extrathoracic airways diminish in caliber during inspiration due to their intraluminal pressure being lower than the atmospheric pressure. The reverse happens during expiration.
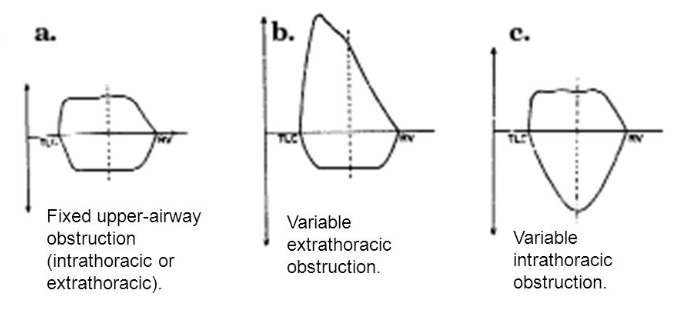
- Flow volume loop inupper-airway obstruction:
- Fixed lesions[extrathoracic or intrathoracic] are characterized by lack of changes in caliber during inhalation or exhalation and produce a constant degree of airflow limitation during the entire respiratory cycle. Its presence results in similar flattening of both the inspiratory and expiratory portions of the flow-volume loop
- Variable lesions are characterized by changes in airway lesion caliber during breathing. Depending on their location (intrathoracic or extrathoracic), they tend to behave differently during inhalation and exhalation.
- In the case of an extrathoracic obstructing lesion, during inspiration, there is acceleration of airflow from the atmosphere toward the lungs, and the intraluminal pressure decreases with respect to the atmospheric pressure due to a Bernoulli effect, resulting in the limitation of inspiratory flow seen as a flattening in the inspiratory limb of the flow-volume loop. During expiration, the air is forced out of the lungs through a narrowed (but potentially expandable) extrathoracic airway. Therefore, the maximal expiratory flow-volume curve is usually normal.
- Variable intrathoracic constrictionsexpand during inspiration, causing an increase in airway lumen and resulting in a normal-appearing inspiratory limb of the flow-volume loop. During expiration, compression by increasing pleural pressures leads to a decrease in the size of the airway lumen at the site of intrathoracic obstruction, producing a flattening of the expiratory limb of the flow-volume loop
An anesthesiologist is a person, standing at the interface of medical and surgical specialties. He may cease to be an expert outside his field; but still possess a bird’s eye view of most specialties. So I would like to label him as a 'layman' among the various specialists, who can save lives. This blog contains, easy to read snippets of info from his world i.e. Anesthesiology
Tuesday, October 2, 2018
MEDIASTENAL TUMOURS & THE ANESTHESIOLOGIST: SPECIFIC POINTS
Subscribe to:
Post Comments (Atom)
No comments:
Post a Comment